Different Types Of Psoriasis
Table of Contents
Psoriasis is a chronic autoimmune condition that can present in various forms, each with distinct characteristics and symptoms. While all types of psoriasis involve an abnormal immune response leading to rapid skin cell turnover, the specific manifestations can vary widely. Understanding the different types of psoriasis is crucial for accurate diagnosis and effective treatment. Below, we explore the main types of psoriasis, providing an overview of their unique features.
For more detailed information on each type, you can visit the NIAMS Psoriasis page.
Who is most prone to psoriasis?
Psoriasis can affect anyone, but certain factors can increase the likelihood of developing the condition. Here’s a general overview of who gets psoriasis:
Genetic predisposition
Psoriasis often runs in families, suggesting a genetic component. If you have one parent with psoriasis, you have a higher risk of developing the condition. This risk increases further if both parents are affected.
Age
Psoriasis can develop at any age, but it most commonly appears between the ages of 15 and 35. However, it can also develop later in life. There is also a second peak occurrence between the ages of 50 and 60.
Sex
Psoriasis affects males and females equally. However, some studies suggest that certain types, like guttate psoriasis, may be more common in children and young adults.
Ethnicity
Psoriasis can affect individuals of any ethnic background, but its prevalence varies among different populations. It is less common in certain ethnic groups, such as the Japanese and Inuit.
Environmental and lifestyle factors
Certain environmental and lifestyle factors can trigger or exacerbate psoriasis in those who are genetically predisposed. These include:
- Infections: Bacterial and viral infections can trigger psoriasis, particularly in children.
- Stress: High stress levels can exacerbate symptoms.
- Obesity: Being overweight increases the risk of psoriasis and its severity.
- Smoking and Alcohol: Both are known to increase the risk and severity of psoriasis.
Autoimmune disorders
Different types of psoriasis
People with other autoimmune disorders, such as rheumatoid arthritis or inflammatory bowel disease, may be more likely to develop psoriasis due to similar underlying immune system dysfunctions.
Psoriasis is a complex condition influenced by a combination of genetic, environmental, and lifestyle factors. For more detailed information, you can visit the NIAMS Psoriasis page and NHS Psoriasis Overview.
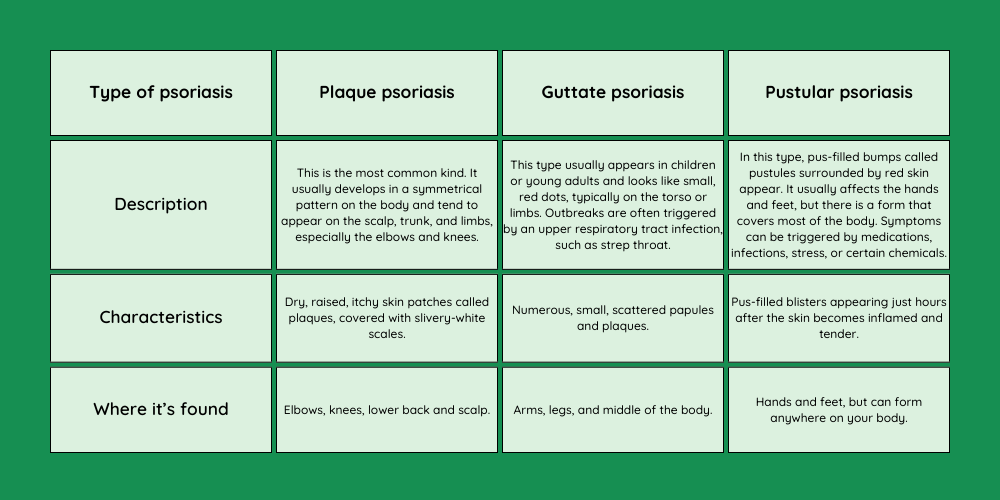
Plaque psoriasis
Plaque psoriasis, also known as psoriasis vulgaris, is the most common form of psoriasis, accounting for approximately 80-90% of cases. It is characterized by:
- Appearance: Raised, inflamed, red lesions covered with silvery-white scales. These plaques are often itchy and can sometimes be painful.
- Location: Commonly found on the elbows, knees, scalp, and lower back. However, they can occur anywhere on the body.
- Symptoms: In addition to the visual and tactile symptoms, affected areas may crack and bleed, particularly in severe cases.
- Triggers: Factors that can exacerbate plaque psoriasis include stress, skin injuries, infections, and certain medications.
The exact cause of plaque psoriasis involves a combination of genetic predisposition and immune system dysfunction, where T-cells mistakenly attack healthy skin cells, leading to rapid cell turnover and the formation of plaques.
For more detailed information on plaque psoriasis and other types, visit the NIAMS Psoriasis page and NHS Psoriasis Overview.
Symptoms of psoriasis
Psoriasis is characterized by a variety of symptoms, which can vary in severity and presentation depending on the type of psoriasis and the individual. Common symptoms include:
Plaques and scales
- Plaques: The most recognizable symptom of psoriasis is the presence of red, inflamed patches of skin, known as plaques. These are often covered with a silvery-white buildup of dead skin cells called scales.
- Location: Plaques commonly appear on the elbows, knees, scalp, and lower back but can develop anywhere on the body.
Itching and pain
- Many people with psoriasis experience itching, burning, or soreness around the affected areas. The severity of these sensations can vary, sometimes leading to significant discomfort.
Dry and cracked skin
- The skin affected by psoriasis can become dry and prone to cracking, which may bleed. This is particularly common in areas of thick plaque buildup.
Nail changes
- Nail psoriasis: This can lead to pitting (small dents in the nails), discoloration, and thickening of the nails. In severe cases, nails may become loose and separate from the nail bed (onycholysis).
Joint pain
- Psoriatic arthritis: Some individuals with psoriasis may also develop psoriatic arthritis, which involves swollen and painful joints. This condition can affect any joint in the body and can range from mild to severe.
Different manifestations by type
- Guttate psoriasis: Characterized by small, drop-shaped sores on the trunk, limbs, and scalp, often triggered by a bacterial infection like strep throat.
- Inverse psoriasis: Causes smooth, red patches of skin that worsen with friction and sweating, typically found in skin folds like the armpits, groin, and under the breasts.
- Pustular psoriasis: Marked by white pustules (blisters of noninfectious pus) surrounded by red skin, which can be localized or widespread.
- Erythrodermic psoriasis: A rare and severe form that can cover large areas of the body with a red, peeling rash that can itch or burn intensely.
Psoriasis symptoms can fluctuate, often improving and worsening in cycles. Flare-ups can be triggered by factors such as stress, skin injury, infections, and certain medications.
For more detailed information, please visit NHS Psoriasis Symptoms and NIAMS Psoriasis Overview (nhs.uk) (nhs.uk).
Causes of psoriasis
The exact cause of psoriasis is not fully understood, but it is believed to result from a combination of genetic, immune system, and environmental factors. Here’s an overview of the primary causes:
Immune system dysfunction
Psoriasis is an autoimmune disorder, meaning the immune system mistakenly attacks the body’s own tissues. In psoriasis, T-cells, a type of white blood cell, become overactive. These cells normally protect the body against infections and disease, but in psoriasis, they mistakenly target healthy skin cells, triggering an inflammatory response. This response accelerates the growth cycle of skin cells, causing them to accumulate on the surface of the skin and form plaques (nhs.uk) (nhs.uk).
Genetics
There is a strong genetic component to psoriasis. Research has identified several genes associated with the disease, suggesting that a predisposition to psoriasis can be inherited. If one or both parents have psoriasis, there is an increased likelihood that their children will develop the condition. However, having the genetic predisposition does not guarantee that a person will develop psoriasis, indicating that other factors play a role (nhs.uk).
Environmental triggers
Environmental factors can trigger the onset of psoriasis or exacerbate its symptoms. These triggers include:
- Infections: Infections, particularly streptococcal throat infections, can trigger psoriasis flares, especially in children and young adults.
- Skin injuries: Cuts, scrapes, bug bites, or sunburn can trigger a psoriasis flare, a phenomenon known as the Koebner response.
- Stress: Emotional stress can worsen psoriasis symptoms by affecting the immune system.
- Climate: Cold, dry weather can aggravate psoriasis, while warm, sunny climates may help reduce symptoms.
- Medications: Certain medications, such as lithium, beta-blockers, and antimalarial drugs, can trigger or worsen psoriasis.
Lifestyle factors
Lifestyle choices such as smoking and heavy alcohol consumption are known to exacerbate psoriasis symptoms and may contribute to the development of the condition.
For more comprehensive information, you can visit NHS Psoriasis Causes and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) (nhs.uk).